By MICHELLE ROBERTS
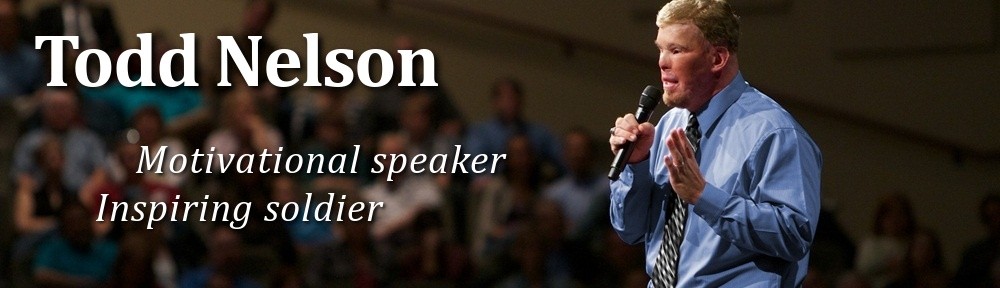
SAN ANTONIO — Master Sgt. Todd Nelson lost his right eye and ear in a flash when a car bomb in Afghanistan exploded, sending fire up his arm and over his head.
Although it’s taken years of painstaking work, the military has given him a bright blue eye and ear lightly freckled and pinked from summer sun. They’re not flesh and blood, but the glass and silicon replicas are so realistic, so perfectly customized, that they’ve given Nelson something else: the ability to face the world without shocking it.
“Honestly, people really don’t know it’s artificial,” said Nelson, whose injuries three years ago included third-degree burns, a skull fracture and broken jaw. “In casual social interactions, I see much smaller cases where people stare.”
The wars in Iraq and Afghanistan have brought a new kind of patient to the facial prothestics lab at the Lackland Air Force Base: wounded warriors, who have recently suffered heavy burns and multiple traumas. The lab is one of two major facial prosthetic programs in the Defense Department, and it has seen an unprecedented new stream of wounded soldiers.
Before the wars, the 26-year-old lab’s patients were almost exclusively cancer and civilian trauma survivors, but “all of that prepared us for wartime, and that’s really why our department is here,” said lab director Dr. Joe Villalobos.
The lab doesn’t track how many soldiers wounded from the war it’s treated. However, before the wars began in 2001 and 2003, the facility rarely saw combat-related injuries — only an occasional Vietnam-era veteran looking for a new prostheses. Now, partly because the lab is across town from the Army’s only burn center, wounded warriors make up about one-fifth of the roughly 425 patients they treat each year.
While the technology and capabilities at the lab are available in the civilian world, the Lackland lab has the expertise and resources to give soldiers the best possible care with little concern about the financial burdens that civilian trauma patients might face, he said.
“Our goal is to give them the best of the best,” Villalobos said. “We’re going to give them the ideal treatment.”
Patients at Lackland are treated with a combination of cutting-edge technology and carefully hand-hewed prostethics.
Using specially designed computer equipment, technicians can turn an MRI into three-dimensional molds and create custom-fit pieces to replace missing jaw bones or sections of skull for implant. The lab has even done it remotely, creating a perfectly fitting replacement for one-third of a patient’s skull at a hospital in Balad, Iraq, Villalobos said.
But sometimes, after patients have undergone life-saving surgeries and reconstruction work for basic functionality, aesthetics start to matter. Soldiers tire of stares and flashes of shock on the faces of people unaccustomed to severe burn injuries.
“When your face is affected, you lose your identity,” said Villalobos. “We address that here.”

Not everyone who loses an ear, eye or nose tip is interested in getting a new one. After the memory of what you used to look like begins to fade, “you start to accept who you are,” said Nelson, a 37-year-old Army mechanic from Evergreen, Colorado. And because burn patients typically undergo dozens of surgeries (Nelson is at 43 and counting), many are simply too procedure-weary to seek prosthetic ears or noses.
But Nelson said for him, “one of the things that bothered me the most aesthetically was the missing ear.”
He knew getting a prosthetic right ear, sculpted to match his remaining ear on the left, wouldn’t make a functional difference. If anything, the prosthetic has slightly dampened noises.
“It was for form, but I couldn’t help but want some of my form back,” said Nelson, who sometimes wears a hair piece to cover his burned scalp.
To create prosthetic ears, the lab uses cameras that generate 3-D images for technicians to make molds. While adhesive can be used to keep prosthetic ears in place, younger patients like Nelson often opt for titanium implants that allow the prosthetic to magnet on.
When a patient has one ear remaining, a mirror-image ear is created. Two missing ears are more difficult, said Villalobos, but the lab has created ears using family members as models.
One soldier wanted his father’s ears, so the lab took images and created versions that were smaller and less wrinkly to make sure the prosthetic versions were right for the soldier’s age, Villalobos said.
The technicians pay close attention to detail.
Nancy Hanson, the lab’s clinical anaplastologist, carefully matches skin tone using powdered pigment and tiny red and blue embroidery threads to create the visual effect of veins. Freckles are painted on, and tops of ears are pinked to mimic sun exposure. Some soldiers get “summer ears” and “winter ears” to account for skin-tone variation.
“It’s a combination of a little bit of science, art and ingenuity,” said Hanson. “We deal with very unique situations.”
Nelson’s ear took about two years to complete, in part because his caregivers had to fight growth of scar tissue that kept covering the titanium implants and creating uneven skin on the side of his head.
Nelson said he was shocked at how realistic the fake ear turned out even after going through multiple fittings and coloration sessions to match his skin tone and freckles.
“I do feel like I have the best-looking one ever made,” he smiled.